Multiple Sclerosis (MS)
Multiple sclerosis (MS) is a complex and one of the more common demyelinating disease of the central nervous system (CNS).
Multiple sclerosis (MS) is a complex demyelinating disease in the central nervous system (CNS) that causes loss of the insulating sheath of the nerve fibers, thereby disrupting information transmission between the brain and the body. MS patients often suffer from serious disabilities impacting movement, vision, sensation, cognition, ambulation, and balance. Depending on the disease progression, MS is categorized into three major forms: Relapsing-Remitting MS (RRMS), Secondary Progressive MS (SPMS), and Primary Progressive-relapsing MS (PPMS).
Current Treatment
MS is still considered incurable. Available treatments are mainly focused on facilitating recovery from relapses and slowing disability progression, management of symptoms and rehabilitation. Currently, there have been almost 20 agents approved for MS treatments, many of which have varying degrees of short and long-term adverse effects causing discomfort and suffering in patients; such as injection site reactions, flu-like symptoms, bradycardia, macular edema, diarrhea, alopecia, lymphopenia, and opportunistic infections.
T-MSC (hES-MSC) as a Potential Stem Cell Medicine for MS
ImStem has discovered that hESC-MSCs display improved immunomodulatory abilities and lower propensity for immunogenicity when compared to MSCs derived from adult bone marrow (BM-MSC). Moreover, in the brain of MS mouse model, hES-MSCs displayed fewer CD4+, CD8+, Th1 and Th17 T cell infiltration compared to BM-MSCs, suggesting lower immune-mediated inflammation. The unique feature may be explained by our observations that hESC-MSCs secrete much less pro-stimulatory cytokines and express much lower amount of major MHC-II antigens. With these properties, hESC-MSCs may work as a potential treatment for MS via modulating immune-mediated inflammation, slowing disease progression, supporting remyelination and restoring functions.
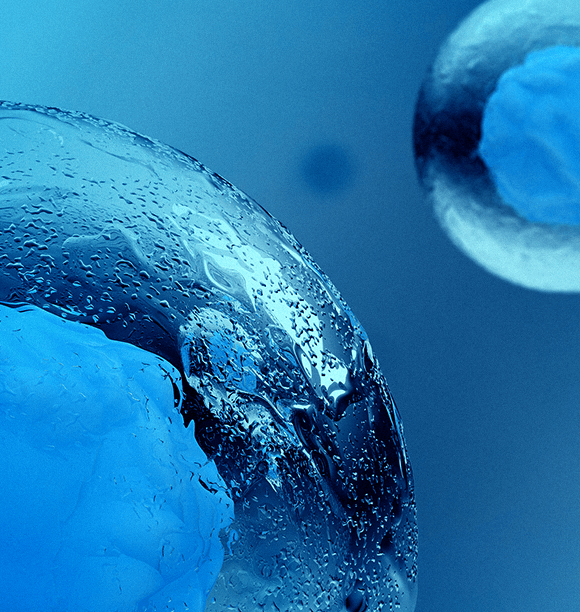
Scientific investigations conducted by Dr. Xiaofang Wang and his team in 2014 have demonstrated that hES-MSCs outperform BM-MSCs in the treatment of an EAE (experimental autoimmune encephalomyelitis) model of MS. In an experiment where hESC-MSC and BM-MSCs from different donors were given to MS mice of an EAE model group as a prophylactic treatment, hES-MSCs significantly further attenuated the disease scores compared to BM-MSCs. This beneficial effect is consistent, as hES-MSCs were able to reduce EAE disease scores in mice from the MS group regardless of whether hES-MSC was administered as a prophylactic or therapeutic treatment. Findings concluded hESC-MSC effectively prevented demyelination in MS mice of an EAE model group.
ImStem has carried out extensive pre-clinical pharmacology, pharmacokinetics, and toxicology studies to determine the potential for T-MSCs in treating MS. EAE MS disease models were selected as the main animal model in our preclinical studies. We have completed pre-clinical studies on T-MSC biodistribution, engraftment, tumorigenicity, toxicology, and immunogenicity. Based on these studies, ImStem has received FDA Investigational New Drug (IND) clearance to proceed with our clinical trials investigating IMS001, the first T-MSC platform cell product, in treating MS patients. IMS001 is the first hES-MSC, intravenously delivered, allogeneic off-the-shelf stem cell therapy accepted by the FDA, for clinical trials, to proceed in MS patients.
